'Save your thyroid'
 Home >
Solutions - Microwave Ablation - MWA in Thyroid
Home >
Solutions - Microwave Ablation - MWA in Thyroid
Thyroid cancer is responsible for 586,000 cases worldwide, ranking in 9th place for incidence in 2020. The global incidence rate in women of 10.1 per 100,000 is 3-fold higher than that in men. Mortality rates from the disease are much lower, with rates of 0.5 per 100,000 in women and 0.3 per 100,000 in men and an estimated 44,000 deaths in both sexes combined [1].
According to 2020 European Thyroid Association Clinical Practice Guideline and European Thyroid Association and Cardiovascular and Interventional Radiological Society of Europe 2021 Clinical Practice Guideline, due to the frequent indolent nature, cost, and risk of surgery, image-guided thermal ablation (TA) procedures like microwave ablation has been proposed as non-surgical treatment options for around 3 decades [2][3].
As an alternative option, Image guided Microwave Ablation technology has been widely recommended and used as clinical treatment for thyroid diseases. It is mainly indicated for the treatment of thyroid nodules and thyroid cancers like papillary thyroid microcarcinomas (PTMCs).
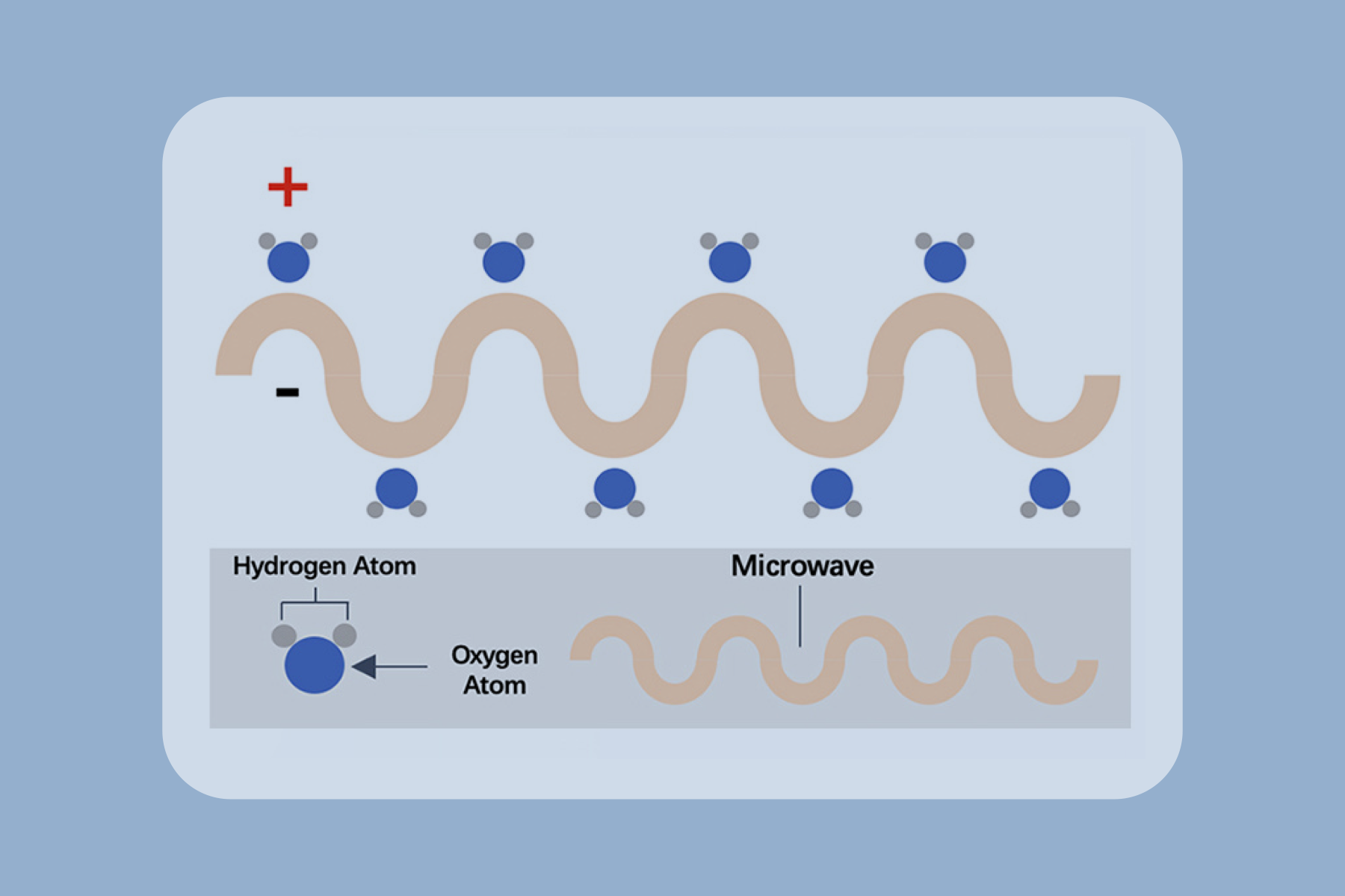
Microwave ablation refers to the use of the electromagnetic methods for inducing tumor destruction by using devices with frequencies of at least 900 MHz to produce tissue-heating effects [4]. Currently, 2450MHz is the frequency used by mainstream products worldwide.
The first studies were reported by Chinese researchers. Feng et al. first demonstrated the feasibility of MWA to treat benign thyroid nodules and reported a mean volume reduction rate of 45.9% (from 1 to 9 month) [6].
A study involved 198 patients with T1NOMO mETE-PTCs (92 patients elected MWA and 106 patients elected surgery for treatment) were included to assess the rates of technical success, oncologic outcomes, complications, and quality of life. The follow-up times for the MWA and surgery groups were 12.7 ± 4.1 and 12.6 ± 5.0 months, respectively. The technical success rate was 100% for both groups. Oncological outcomes of the two groups were similar during the follow- up. Three complications (3.3%) were reported in the MWA group and 4 (3.8%) in the surgery group. The surgery group had higher scores for scar problems and anxiety [7].
A study evaluated 171 patients with 180 benign thyroid nodules (BTNs) that had been treated with ultrasound guided MWA. The mean diameter and volume of the nodules were 4.3 ± 1.3 cm and 18.9 ± 2.1 ml, respectively. The VRRs at the 1-, 3-, 6-, 12-, 24-, and 36-month follow-ups were 47.1%, 68.2%, 79.7%, 87.4%, 90.1%, and 93.2%, respectively [8].
In conclusion, the ultrasound-guided MWA is an effective and safe procedure for the treatment of benign thyroid nodules and PTMC.
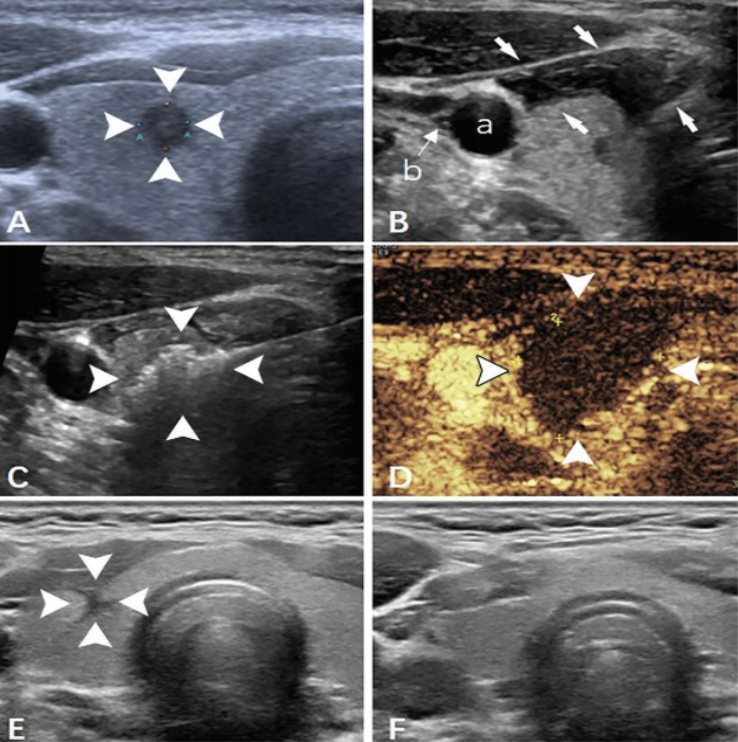
US images in a 36-year-old man with papillary thyroid carcinoma in the right lobe of the thyroid [9]. (A) Preablation image of the tumor (arrowheads). (B) The hydrodissection technique (arrows) was used to protect the carotid artery (a) and vagus nerve. (C) Hyperechoic pattern in the tumor during the ablation procedure(arrowheads). (D) Postablation contrast-enhanced image shows no enhancement in the tumor area (arrowheads). (E) Image of the ablation zone 6 months after ablation (arrowheads). (F) The ablation area has almost disappeared 1 year after ablation.
Advantages
High cosmetic score and less scarring

Shorter hospitalization stay

Little to no damage to healthy thyroid tissue, preserving the thyroid functions
Quicker recovery time

High success rate with low risk of complication
General anesthesia is not required
1. Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, ., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 71(3), 209-249.
2. Papini, E., Moneyssen, H., Frasoldati, A., & Hegedüs, L. (2020). 2020 European thyroid association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. European thyroid journal, 9(4),172-185.
3. Mauri, G., Hegedüs, L., Bandula, S., Cazzato, R. L., Czarniecka, A., Dudeck,O. & Papini, E. (2021). European Thyroid Association and Cardiovascular and Interventional Radiological Society of Europe 2021 clinical practice guideline for the use of minimally invasive treatments in malignant thyroid lesions. European thyroid journal, 10(3), 185-197.
4. Simon, C. J., Dupuy, D. E., & Mayo-Smith, W. W. (2005). Microwave ablation: principles and applications. Radiographics, 25(suppl_1), S69-$83.
5. Xu, B., Zhou, N. M., Cao, W. T., & Gu, S. Y. (2018). Comparative study on operative trauma between microwave ablation and surgical treatment for papillary thyroid microcarcinoma. World Journal of Clinical Cases, 6(15), 936.
6. Feng B, Liang P, Cheng Z, et al. (2012). Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: experimental and clinical studies. Eur J Endocrinol 166:1031-37.
7. Zheng, L., Dou, J. P., Liu, F. Y., Yu, J., Cheng, Z. G., Yu, x. L., ... & Liang, P. (2023). Microwave ablation vs. surgery for papillary thyroid carcinoma with minimal sonographic extrathyroid extension: a multicentre prospective study. European Radiology, 33(1), 233-243.
8. Luo, F., Huang, L., Gong, X., Han, Z., Liu, F., Cheng, Z., ... & Yu, J. (2021). Microwave ablation of benign thyroid nodules: 3-year follow-up outcomes. Head & Neck, 43(11), 3437-3447.
9. Zheng, L., Dou, J. P., Han, Z. Y., Liu, F. Y., Yu, J., Cheng, Z. G., ... & Liang, P. (2023). Microwave Ablation for Papillary Thyroid Microcarcinoma with and without US-detected Capsule Invasion: A Multicenter Prospective Cohort Study. Radiology, 307(3), e220661.








