 Home >
Solutions - Microwave Ablation - MWA in Lung
Home >
Solutions - Microwave Ablation - MWA in Lung
Approximately, 2.2 million new cases of lung cancer and 1.8 million lung cancer related deaths were reported in 2020 worldwide. Although the incidence of lung cancer ranks the second in the world, the mortality rate is the highest [1].
By 2022, China and the USA are expected to have approximately 870,982 and 238,032 new lung cancer cases, and 766,898 and 144,913 lung cancer deaths, respectively [2].
For early-stage NSCLC, surgical resection with curative intent comprises the primary therapy, however, approximately 60% of lung cancers cannot be resected surgically due to various reasons. Therefore, microwave ablation, a precise minimally invasive technique, has been applied on treating early-stage lung cancer [3].
As an alternative option, Image guided Microwave Ablation technology has been widely recommended and used as clinical treatment for lung diseases. According to the Lung Clinical Practise Guidelines [3] and Expert Consensus [4], It’s mainly indicated for the treatment of pulmonary subsolid nodules as well as primary and metastatic lung tumors.
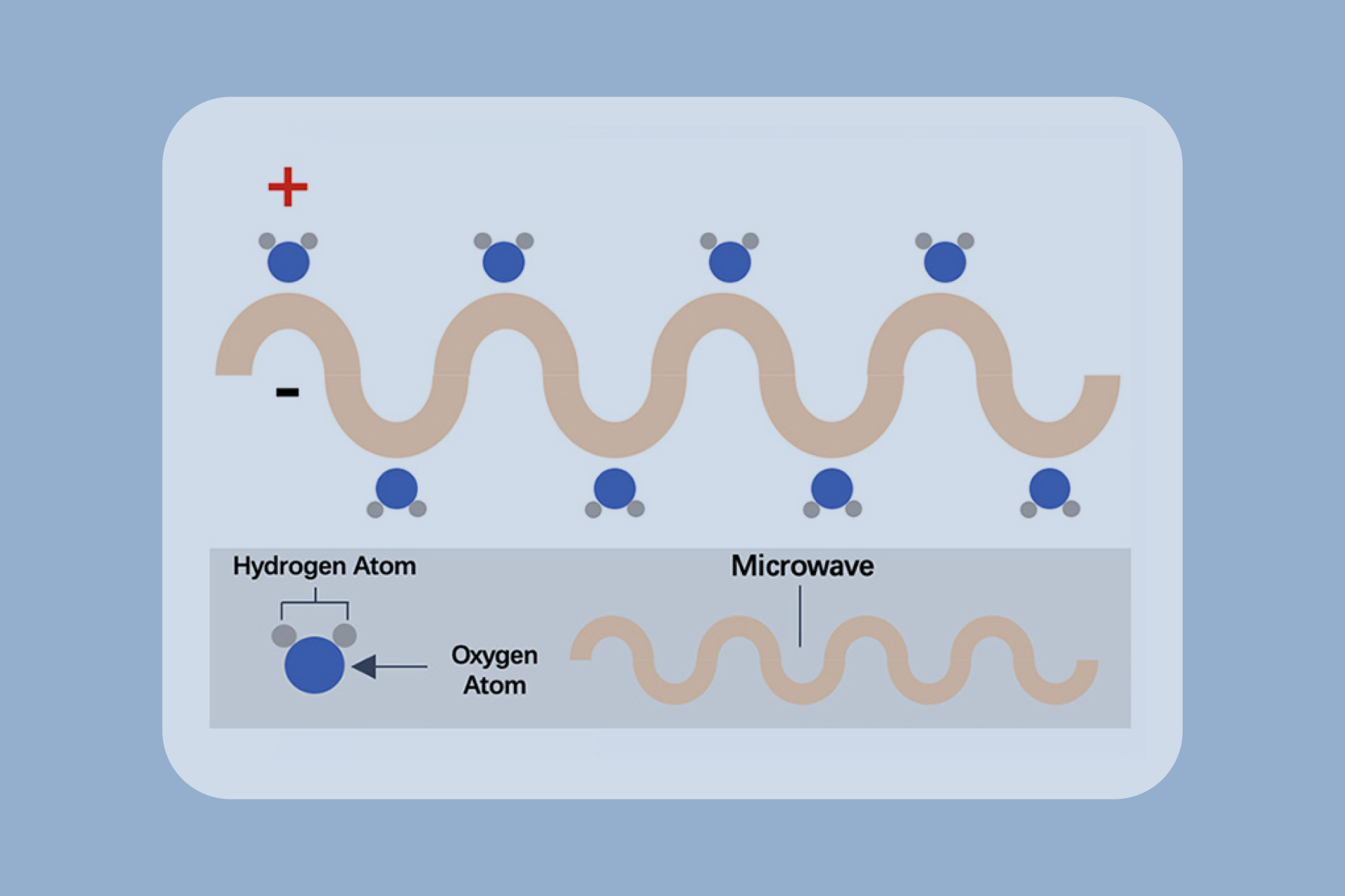
Microwave ablation refers to the use of the electromagnetic methods for inducing tumor destruction by using devices with frequencies of at least 900 MHz to produce tissue-heating effects [5]. Currently, 2450MHz is the frequency used by mainstream products worldwide.
MWA for the treatment of lung cancer was first attempted in 2002 in China, using computed tomography (CT) guided imaging [3].
A study involved 33 patients with multiple GGOs (103 GGOs with mean size 12.3 ± 6.3 mm) underwent 66 procedures of CT-guided percutaneous MWA. The technical success and technique efficacy rate were 100%. The median follow-up period was 18.1 months. During the follow-up, there was no local tumor progression, tumor recurrence, or death among the 33 patients [6].
Another study involved 105 patients proven clinical stage I NSCLC were treated with CT-guided MWA. The mean age was 70.7 years, and the mean diameter of all lesions was 2.40 cm. Adenocarcinoma was the most common histological type (77, 73.3%), followed by squamous cell carcinomas (21, 20%) and undefined NSCLC (7, 6.7%). With a median follow-up of 54.8 months, the median overall survival (OS) was 64.2 months. The OS rate was 99% at 1 year, 75.6% at 3 years, and 54.1% at 5 years [7].
In conclusion, MWA is a safe, effective, and potentially curative therapy for GGO and stage I NSCLC patients that are not suitable for surgical resection.

CT of an 80-year-old woman with right upper lobe adenocarcinoma at stage IA (cTlaNOMO). (a) The MWA antenna is shown centrally positioned within the tumor [8]. (b) Ground-glass opacity around the tumor and cavity ni the core was observed ni the image obtained immediately postablation. (c) The axial CT with lung window showed expected thermal damage around the target lesion, without pneumothorax, 24 hours postablation. (d) The enhanced CT image at one month after MWA; the size of the ablation zone was larger than the target tumor but was not enhanced. (e-g) The images at six, 12, and 91 months after MWA; the ablation zone shrank continuously and remained nonenhanced.
Advantages
Reduce morbidity and mortality

Suitability for imaging guidance

Shorter hopitalization stay

Synergy with other cancer treatments

Repeatability
Cost effectively

1. Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 71(3), 209-249.
2. Xia, C., Dong, X., Li, H., Cao, M., Sun, D., He, S., ... & Chen, W. (2022). Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chinese medical journal, 135(05), 584-590.
3. Ye, X., Fan, W., Wang, Z., Wang, J., Wang, H., Niu, L., ... & Roy, S. H. (2022). Clinical practice guidelines on image-guided thermal ablation of primary and metastatic lung tumors (2022 edition). Journal of Cancer Research and Therapeutics, 18(5), 1213-123.
4. Ye, X., Fan, W., Wang, Z., Wang, J., Wang, H., Wang, J., ... & Pan, J. (2021). Expert consensus on thermal ablation therapy of pulmonary subsolid nodules (2021 Edition). Journal of Cancer Research and Therapeutics, 17(5), 1141-1156
5. Caroline J. Simon., Damian E. Dupuy., William W. Mayo-Smith., Microwave Ablation: Principles and Application. RadioGraphics 2005; 25:S69–S83
6. Huang, G., Yang, X., Li, W., Wang, J., Han, X., Wei, Z., ... & Ye, X. (2020). A feasibility and safety study of computed tomography-guided percutaneous microwave ablation: a novel therapy for multiple synchronous ground-glass opacities of the lung. International Journal of Hyperthermia, 37(1), 414-422.
7. Ni, Y., Huang, G., Yang, X., Ye, X., Li, X., Feng, Q., ... & Wei, Z. (2022). Microwave ablation treatment for medically inoperable stage I non-small cell lung cancers: Long-term results. European Radiology, 32(8), 5616-5622.
8. Han, X., Yang, X., Huang, G., Li, C., Zhang, L., Qiao, Y., ... & Ye, X. (2019). Safety and clinical outcomes of computed tomography‐guided percutaneous microwave ablation in patients aged 80 years and older with early‐stage non‐small cell lung cancer: A multicenter retrospective study. Thoracic cancer, 10(12), 2236-2242. 5








